A Guide to Massage Billing: Insurance Codes for Therapists
- Kyle Cannon
- August 15, 2023
- - Practice management

Although many people receive massages for relaxation, some individuals need massage therapy for medical reasons. If you’re interested in receiving these clients, then you’ll want to know more about massage billing, specifically about how medical insurance intersects with the massage therapy industry.
In this guide, we’ll cover the following topics to help you learn more about massage billing and insurance:
- Massage Billing FAQs
- 5 tips for avoiding massage billing delays and denials
- How software helps with massage billing
Venturing into the medical world can be overwhelming, as there are many rules and regulations that you need to stay informed about and remain compliant with. This article will guide you through the basics of massage billing and medical insurance and help you evaluate whether accepting insurance for massage billing is the right move for your practice. Let’s begin!
Massage Billing FAQs
Should I accept insurance coverage for massage billing?
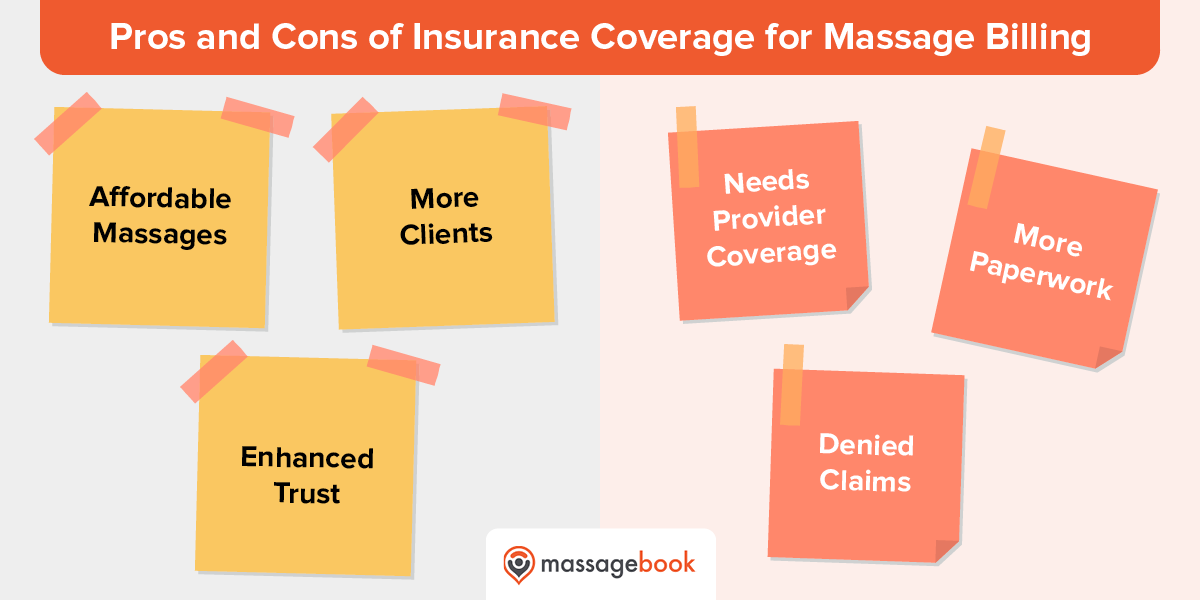
There are many benefits to accepting insurance coverage for massage billing, such as:
-
Makes massages more affordable. Some individuals who need medical massage care may not be able to afford them out of pocket. If your practice is able to accept their medical insurance, then massages will be more accessible to those clients.
-
Increases traffic to your massage practice. Because you’ll be making massages more affordable for your clients, it will increase the traffic to your practice, resulting in an increased amount of bookings. Plus, you’ll be more likely to retain your clients, as not every massage provider will accept their insurance.
-
Enhanced trust and credibility. By accepting health insurance, your practice will essentially be offering healthcare services. This will enhance your clients’ trust in your practice to deliver high-quality massage therapy. And, you’ll be able to differentiate your business from others by highlighting this in your promotional materials.
While accepting medical insurance payments offers many advantages, it also comes with some downsides. When deciding if you should accept insurance for massage billing purposes, consider the following:
-
Massage therapy insurance coverage. Not all insurance providers cover massage therapy. Research the most common insurance providers in your area and find out if they cover massages. If not, then it may not be worth it for you to accept insurance.
-
Insurance paperwork. Medical insurance can complicate the massage billing process, as it requires you to fill out paperwork. To successfully incorporate medical insurance into your massage billing processes, you’ll need to have the ability to manage extra paperwork on top of your existing responsibilities.
-
Payment uncertainty. It’s possible that an insurance provider may deny a claim that you file. In that case, you may not receive all of the payment you billed for. You’ll need to either bill your patient for the remaining balance or accept the partial payment for your services.
It’s up to you to determine if the benefits outweigh the costs for your unique practice. However, if you find that not many providers in your area cover massage therapy, you’re unable to keep up with your existing paperwork, and you’re not willing or able to put in the effort to ensure you get paid the correct amount, then perhaps accepting insurance is not the right move for your business.
What do you need to accept massage billing insurance?
To accept medical insurance, you’ll need a variety of different qualifications and documents. These will vary depending on local or state laws, but in general, you will need the following:
- License to practice massage therapy
- National Provider Identifier (NPI)
- Prescription for massage therapy
- Current Procedural Terminology (CPT) codes
- Detailed SOAP (Subjective, Objective, Assessment, and Plan) treatment notes
Before you begin accepting medical insurance, double-check with your massage practice board and ask them any questions you have about insurance billing and how massages are generally covered in your area. Additionally, you’ll want to have a system in place for collecting and storing information about the massage sessions you provide. This is to help support your payment request by proving that you provided a service to your clients.
What are the common CPT codes for massage billing?

CPT codes are created by the American Medical Association (AMA) to give structure to procedures and services performed by healthcare providers. They are also used for administrative purposes, such as insurance claims processing.
The CPT codes most relevant for massage billing include:
-
97010: Hot and Cold Pack Therapy. This code describes the application of any physical agent to produce therapeutic changes to biologic tissue. Most commonly, it describes the application of moist heat, cryotherapy, or hydrotherapy. Many insurance providers consider this code a “bundled” service, which means that reimbursement for this code is grouped with reimbursement for another code. This code is not time-based and may only be billed once per day, so if your client has received this type of therapy from another medical practitioner, then you will not be able to use this code.
-
97124: Massage Therapy. This CPT code describes a therapeutic massage procedure in one or more areas. It includes effleurage, petrissage, and tapotement. This code is time-based and is billed in increments of 15 minutes. Although this code is similar to 97140: Manual Therapy, keep in mind the intent of your massage. If you’re trying to increase circulation and tissue relaxation, then you would bill 97124: Massage Therapy to the insurance provider. It’s important to note that insurance providers tend to heavily scrutinize the use of massage and will only cover it when medically necessary. For example, if your patient has paralyzed musculature, excessive fluids in the interstitial spaces or joints, or abnormal adherence of tissue to surrounding tissue, then massage therapy may be deemed medically necessary.
-
97140: Manual Therapy. This code describes manual therapy techniques, including mobilization, manipulation, manual lymphatic drainage, and manual traction, in one or more regions. This code is time-based and is billed in increments of 15 minutes. Unlike code 97124: Massage Therapy, 97140: Manual Therapy describes therapy that increases active pain-free range of motion, increases the extensibility of myofascial tissue, and facilitates the return to functional activities. Note that you can only report codes 97124 and 97140 in the same session if you apply the different massage techniques to different areas of the patient’s body.
There are also some CPT codes that seem related to massage therapy, but using them can actually get your claim rejected. Of note are codes 97110: Therapeutic Exercise and 97112: Neuromuscular Re-education. These codes are meant for physical therapists, so if you’re not trained or licensed as a physical therapist, your claim will most likely be denied.
In addition, you may need to clarify the intent and activity of your massage services by using a CPT code modifier. For example, CPT code modifier -59: Distinct Procedural Service is used to identify two procedures of a similar nature performed on the same individual on the same day or within a few days.
If you’re reporting codes 97124: Massage Therapy or 97140: Manual Therapy alongside evaluation and management codes or chiropractic manipulation treatment codes, then you’ll need to append these codes with -59 to make it clear that the massage services you’ve provided are separate from other services performed on the same day. However, using this modifier may raise flags with an insurance company and result in delayed payment.
5 tips for avoiding massage billing delays and denials
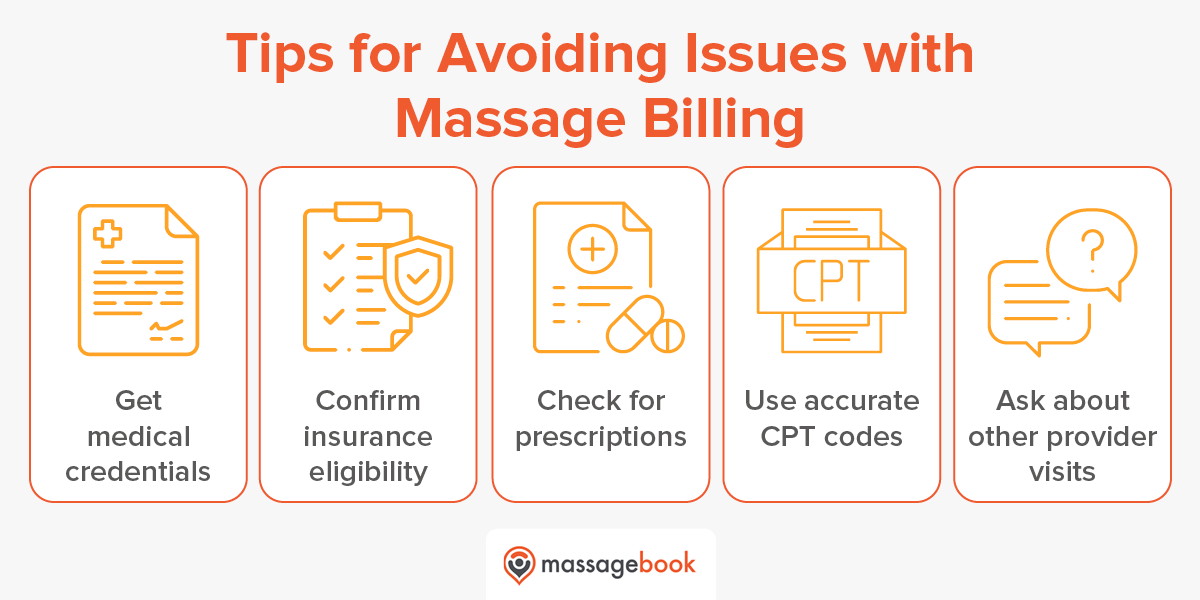
While delays and denials are a definite drawback of accepting insurance at your practice, there are ways you can mitigate this limitation. Here are five tips to avoid delays and denials for your massage billing:
-
Get medical credentials for your practice. To accept insurance at your massage practice, you’ll need to meet medical credentialing requirements. While not all insurance companies require this, many do, so it’s a good idea to collect the necessary documentation and licenses and get them verified.
-
Confirm insurance eligibility before appointments. A common issue with massage billing, or any type of medical billing, is that claims will be delayed or denied because of issues with a patient’s insurance coverage. To prevent this issue, confirm your clients’ insurance eligibility before appointments. This will help ensure that you receive payment for your services.
-
Ensure that patients have massage therapy prescriptions. Since insurance providers usually only cover massage therapy if it’s medically necessary for your client, you’ll need to check that patients have a medical prescription or referral for massage therapy from a physician. This will include a start date, number of visits, frequency of sessions, and diagnosis codes referencing the patient’s injury or condition. You can also use this information to begin forming a treatment plan for your patient.
-
Use accurate CPT codes when billing. The AMA annually updates its codes and regulations, so you’ll need to stay up-to-date with them to ensure streamlined claims processing. Sometimes codes are revised or discarded altogether, so you’ll want to double-check that you’re filing claims with the correct codes.
-
Avoid scheduling massages alongside other provider visits. Due to limitations on certain billing codes related to massage therapy, you’ll want to avoid scheduling massage therapy sessions on the same day that a client has another provider visit. For example, code 97010: Hot and Cold Pack Therapy can only be billed once per day. That means that if your client has received this therapy from another provider on the same day that they visit your practice, you may not be able to receive full reimbursement for your massage services.
Although massage billing is complex, you can facilitate prompt insurance processing by incorporating these strategies. And, you’ll be able to minimize claim denials, ensuring that you receive the appropriate payment for your massage therapy services.
How software helps with massage billing
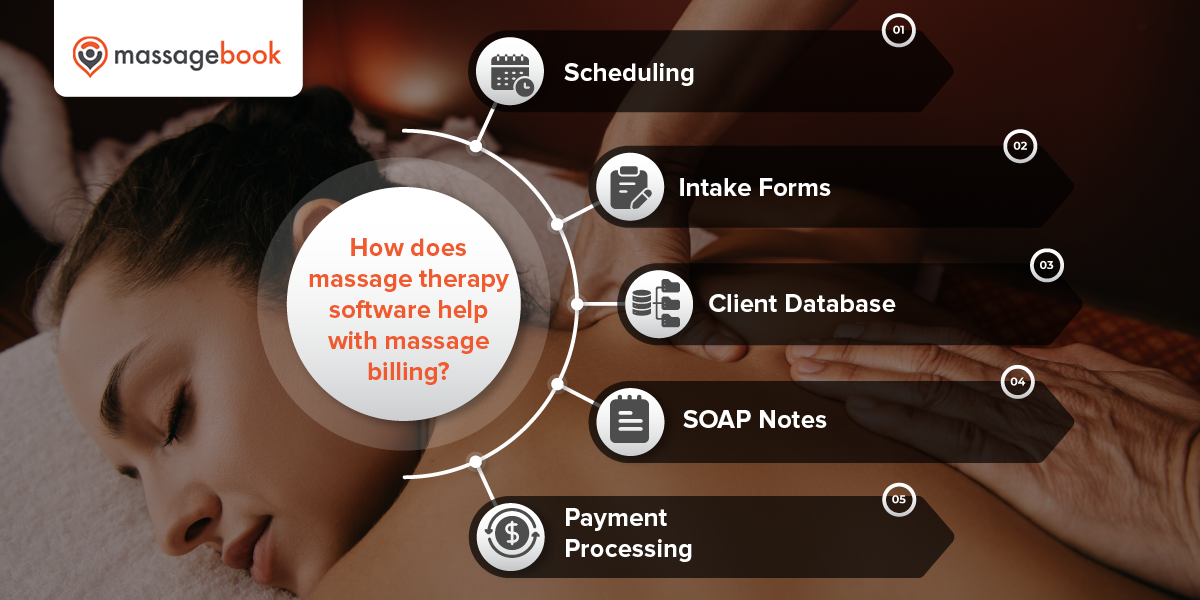
Accepting insurance coverage for massage billing adds extra work to your plate, and as a small business owner, you may feel that this extra effort is not worth the benefits. However, before you completely dismiss the idea, consider that the right massage therapy software solution can be an enormous help for streamlining your massage billing processes.
Some helpful massage therapy software features include:
-
Scheduling. As accepting insurance coverage makes massages more accessible and affordable, you may experience an increase in the number of clients you see. Massage therapy solutions often come with online scheduling capabilities to help you simplify your workflow.
-
Intake forms. Request that clients fill out intake forms online prior to their appointment with massage therapy software. Use these intake forms to ask your clients if they are covering their visit with insurance, verify if they have a prescription or referral, and check if they have another provider visit scheduled on the same day.
-
Client database. Track client-specific information in a single, centralized location. This includes appointment history, contact information, and messages. You can also make a note if your client uses insurance so you’ll know how to handle massage billing for them in the future.
-
SOAP notes. Insurance providers usually require detailed treatment notes when you file a claim. Massage therapy solutions allow you to take in-depth SOAP notes that are secure. Plus, you’ll be able to create a more detailed treatment plan for your clients, helping you provide massages that relieve pain and address their medical needs.
-
Payment processing. With massage therapy software, you can accept a variety of payment methods, including HSA and FSA, and even split payments between different methods. Some solutions also enable you to offer insurance billing receipts, which list specific info for clients who want to submit their receipts to their insurance provider. These receipts include the service date and time and the provider’s name, state license number, and unique NPI number.
Aside from these specific billing-related benefits, massage therapy software is beneficial for your practice in other ways. These solutions can improve client communication, keep your data organized, and even help you acquire and retain clients. Even if you decide not to accept insurance coverage, consider how massage therapy solutions can help streamline your practice’s processes and address your pain points.
Additional Resources
Although massage therapy has historically been overlooked by insurance providers, that attitude is changing, and it’s becoming more and more viable for massage therapists to accept insurance at their practices. However, there are many rules and regulations that can make it difficult for you to add insurance to your massage billing processes. Ultimately, it’s up to you to weigh the benefits and drawbacks and decide whether or not it’s worth it for your practice to make the change.
If you’re interested in learning more about running a massage therapy business, take a look at the following resources:
- 7 Best Massage Therapy Software Solutions for 2023 — Massage therapy solutions help practices in numerous ways, including making insurance billing more convenient. Read our list of the top massage therapy software solutions.
- Why Every Massage Therapist Should Raise Their Prices and How to Do It Without Losing Clients — Raising your prices can be scary. You never know how clients are going to react and you don’t know if they’ll continue to patronize your practice. However, we think it’s worth it, and we’ll teach you to raise your prices without losing your clients.
- SOAP Notes for Massage: A Complete Guide + Free Template — Even if you’re not planning on accepting insurance at your practice, having detailed SOAP notes can help you retain clients by providing exceptional massages. Check out our guide and download our free SOAP notes template!
- Author: Kyle Cannon
- Published: August 15, 2023
Grow and simplify your practice!
Related Posts
Recent Blog Posts
Categories
Categories Index ( 21 )
- Friday focus (9)
- Massage therapists (42)
- Massage therapy benefits (7)
- Marketing (157)
- Massagebook features (12)
- Healthy living (12)
- Press (2)
- Practice management (55)
- From our ceo (3)
- Software releases (23)
- Education (5)
- People focus (3)
- Types of therapy (1)
- Uncategorized (1)
- Massagebook (36)
- Massage therapy (4)
- Massage practice (1)
- Massagebook (1)
- Fun (1)
- Guest blog (1)
- Resources (2)