How to Write SOAP Notes for Massage: A Guide + Free Template
- Kyle Cannon
- September 12, 2023
- - Resources , Practice management
Running a successful massage therapy practice requires more than just great technique. Being organized and efficient is also crucial to providing a great massage experience for your clients. To create that experience, you need thorough and well-organized records of your clients. A central part of these records should be the SOAP notes you take before and after your clients’ sessions.
In this guide, we’ll help you implement massage SOAP notes for your practice by covering the following topics:
- What are SOAP notes?
- Why are SOAP notes important for massage therapists?
- 3 tips for writing more effective massage SOAP notes
- SOAP notes for massage with MassageBook
SOAP notes help massage therapists create treatment plans and track the progress of their clients, ensuring that they provide the best level of service possible. Plus, they’re extremely beneficial if your practice accepts insurance as a billing option or collaborates with other healthcare providers. Let’s get started!
What are SOAP notes?
SOAP notes are a note-taking format that massage therapists and other healthcare workers use to document their client sessions. Having a standardized format helps you to stay consistent and organized and allows you to focus on the most important parts of your massage session.

SOAP is an acronym, and can be broken down into:
- S = Subjective
- O = Objective
- A = Assessment
- P = Plan
Let’s take a deeper look at each part of this acronym.
S = Subjective
The subjective portion of SOAP notes includes the information that the client tells you in his or her own words. It will also describe your impression of the client’s condition. This information is usually gathered in your initial intake interview and may be supplemented by feedback from the client as your treatment progresses.
Common information noted in the subjective section includes:
- Client’s description of the chief complaint (CC)
- Client’s goals regarding their CC
- Relevant medical history, injuries, or other information
- Client’s perception of their progress
If you have repeat clients, be sure to update the subjective section of their notes on how they’re feeling and how it’s changed from their initial status. This will help you stay up-to-date with their treatment.
Subjective example: Client indicates pain in right shoulder that persists when standing and sitting. At-home ice therapy has had no effect. Client rates pain level as 4/10. Client has had a previous shoulder injury from playing basketball.
O = Objective
The objective section of your massage SOAP notes should cover your clinical findings and observable data from observation, palpation, or reassessment tests. Usually, what goes in this section includes:
- Observations from assessment or reassessment
- Progress toward goals based on objective findings
- Details of specific treatments and modalities provided that day
- Observable or palpable response to that day’s massage treatment
In this section, massage therapists commonly note information like:
- Visual-postural analysis
- Limps
- Muscle guarding
- Holding patterns
- Movement inconsistency
- Atrophy
- Hypertrophy
- Bruises
- Abrasions
- Scars
- Swelling
- Redness
- Skin irregularities
- Varicose veins
- Breathing patterns
- Prosthetics
Although it may be tempting to diagnose your client based on the information in this section, keep in mind that the information here should be objective. Be specific with your information and avoid making value judgments or letting bias or personal opinions influence your notes.
Objective example: Client has tightness in the muscles of the neck and shoulders and hunches over when seated. There is also redness on the right shoulder.
A = Assessment
The assessment portion of SOAP notes for massage requires you to detail how the client is progressing through your massage therapy plan. Usually, the following information is included in the assessment section:
- Your clinical opinion about your client’s progress toward treatment goals
- Client’s overall response to the day’s massage treatment
- Any negative reactions to the day’s treatment
- Precautions or pre-existing conditions that may respond negatively to massage therapy
If you accept insurance billing at your massage practice, then this section of your SOAP notes is the most important and will be closely scrutinized. Insurance providers want to know if the client is making progress toward their goals and if they should be reimbursed for this treatment. Ensure that your notes are thorough and include the relevant details that the insurance provider is looking for.
Assessment example: Conducted range of motion tests, significantly improved after treatment. Client reported 0/10 pain after treatment.
P = Plan
The last section for SOAP notes is the plan section, where you describe the massage treatment you intend to implement. This includes long-term treatment plans and lifestyle recommendations. Your notes should include:
- Plan for following visits
- Updated goals
- Recommendations for frequency and duration of massage treatments
- Reassessment reminders
- Client’s self-care plan
- Referrals
- Notes on medication
For the most recent visit, you should include what worked and didn’t work this time, what to focus on next time, and anything missed. You can also add educational recommendations for the client so that they can learn more about relieving their pain.
Plan example: Next week, focus on neck and shoulders and review stretches and self-massage techniques after a long day of standing.
To help you get started with taking SOAP notes at your massage practice, we’ve created a template that you can download for free. Simply enter your email into the form below and you’ll get access to an interactive digital template as well as a printer-friendly version!
Why are SOAP notes important for massage therapists?

Although massage therapists are not always medical providers, their work is adjacent to those of healthcare professionals. After all, they’re providing a service that is intended to help the well-being of their client, regardless of whether it’s to help them relax or relieve pain.
Since medical professionals use SOAP notes, massage therapists should use them too. Here are a few reasons why it’s important for you to take massage SOAP notes:
-
Professionalism. Taking thorough notes demonstrates to clients that you take their health and satisfaction seriously. This builds trust and fosters stronger relationships with clients, improving your practice’s reputation.
-
Client safety. Some of your clients may have preexisting conditions or injuries that make it painful for them to receive massage therapy on certain parts of their bodies. Having a record of these conditions will help you give your clients the care they need.
-
Treatment planning. During the SOAP notes process, you’ll document your client’s specific needs and goals for their massage therapy sessions. You’ll be able to review these notes prior to your client’s next session, allowing you to easily refresh your memory and have a clear idea of what that massage session will look like.
-
Progress tracking. SOAP notes provide a benchmark for your treatment, allowing you to build a historical overview of your client’s treatment and track progress efficiently. If you’ve had a repeat client for a while, update your SOAP notes with any changes. That way, your notes will stay up to date and you’ll know if you need to make any adjustments to your treatment strategy.
-
Communicate with other providers. If your client is seeing you for pain or other medical reasons, they may also be seeing other medical providers. SOAP notes allow you to communicate and coordinate with other healthcare professionals to ensure that your clients receive the care they need.
-
Liability and legal protection. In cases of legal disputes, SOAP notes serve as a record of your client’s sessions. They can be used to demonstrate that you followed proper protocols and standards of care, protecting you from any liability issues.
Massage SOAP notes empower you to maintain a consistent record-keeping process. Plus, because of its consistency, you’ll always know what to write and how to write it, which will save you time and brainpower. Having such a notetaking system in place now will also help you as your practice grows and hires new therapists, as you’ll be able to communicate consistently with each other through your notes.
3 tips for writing more effective massage SOAP notes
To help you write more effective massage SOAP notes that enable you to give your clients the care they need, let’s dive into a few tips!
1. Write timely notes.
To ensure that you capture all the important information, make sure to take notes in a timely manner. This means that you should be taking notes during your intake appointment and immediately after your massage therapy session when the information is still fresh in your mind. If you wait a few hours or even days, then you may forget relevant information.
After you’re done taking your notes, review them carefully to ensure that you’ve recorded all the important information. Don’t be afraid to make corrections or additions if you find any errors or if any key information is missing. For example, if you filled out the subjective and objective sections during your intake appointment, but a few appointments later, the client brings up that they recently hurt their knee, then you’ll want to update your notes to include that.
2. Keep your notes brief but comprehensive.
SOAP notes are, at the end of the day, notes. That means that they should contain key information but not necessarily be a record of everything that happened during your massage session. Although it may seem contradictory, you want your notes to be brief, yet comprehensive.
For example, if you and your client discuss the latest football game during the massage, you should not include this information in your notes. While it may tell you about one of your client’s hobbies, it does not pertain to their care or treatment, and therefore should not be written down. On the other hand, if your client has many health issues they’d like you to be careful of, you should thoroughly document these concerns instead of prioritizing brevity.
Another way you can keep your notes brief is by incorporating abbreviations in them. This strategy can be tricky, as abbreviations are not standardized for massage therapists. Some may even stand for something else for other medical practitioners. However, with that in mind, abbreviations that are consistent across your team of therapists (such as HA for headache or Hx for history) can reduce the time spent on note-taking and make your notes shorter.
3. Create a thorough note-taking process.
Create a note-taking system to standardize your process and ensure nothing falls through the cracks. For example, if you prefer to take notes by hand, you could print out diagrams of the human body and annotate them to indicate exactly where the client is feeling pain or discomfort. Designate a filing system for your notes as well, such as by using individual folders for each client’s notes.
Or, if you wish to write notes digitally, search for a solution that allows you to add your SOAP notes to your client’s digital records. That way, you can easily access your notes before and after each session to reference them, make updates, and provide the best possible client care.
SOAP notes for massage with MassageBook
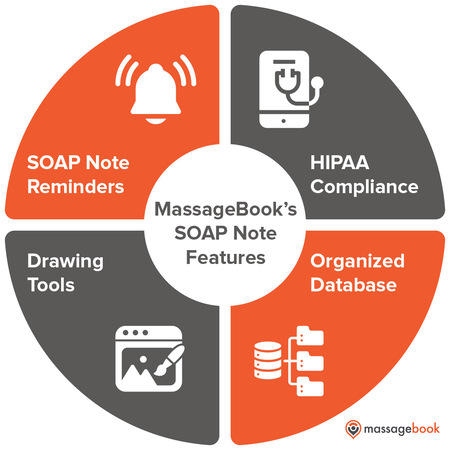
With MassageBook’s massage therapy solution, you’ll have access to faster, more detailed, and more useful SOAP notes for massages. Our solution provides the following features:
-
Organized database. With our client database, not only will you be able to track client activity but also client-specific information, including your SOAP notes. You’ll be able to easily pull up any SOAP notes you need to reference or update before and after your appointments.
-
SOAP note reminders. If you’ve missed writing SOAP notes for any of your clients, our solution will remind you if you’ve missed any. That way, you will remember to take notes that empower you to make your client’s next session more productive.
-
Drawing tools. Annotate your findings directly on an anatomy chart to keep your notes organized and accurate. You’ll have access to a variety of tools and colors to create the perfect visual for your care.
If you’d like to save more time, record professional-quality SOAP notes, and get rid of your paper filing cabinet, now’s a perfect time to explore how MassageBook’s SOAP notes feature can help you reach new levels of productivity. Plus, you can try our premium version free for 30 days! After that, you can even keep using the basic version free for the rest of your first year on MassagBook!
Additional resources
SOAP notes are an extremely useful tool for massage therapists, regardless of whether you’re a single practitioner or you run a larger practice. Hopefully, by now you understand why it’s important for you to use SOAP notes at your practice and how they can help you provide a higher level of care to your clients.
If you’re interested in learning more tips for improving your massage practice, check out the following resources:
- 7 Best Massage Therapy Software Solutions for 2023 — If you’re looking for another way to upgrade your massage practice’s operations, consider investing in massage therapy software. This guide explores the top solutions to consider.
- A Guide to Massage Billing: Insurance Codes for Therapists — Accepting insurance payments for massage therapy has a variety of benefits and drawbacks. Read this article to learn more about whether it’s the right choice for your practice.
- Tips to Help Massage Therapists Simplify Tax Season — Tax season is a daunting time for any business owner, especially if it’s your first time handling your practice’s taxes. Check out our top tips for a smooth tax season.
- Author: Kyle Cannon
- Published: September 12, 2023
Grow and simplify your practice!
Related Posts
Recent Blog Posts
Categories
Categories Index ( 21 )
- Friday focus (9)
- Massage therapists (42)
- Massage therapy benefits (7)
- Marketing (157)
- Massagebook features (12)
- Healthy living (12)
- Press (2)
- Practice management (55)
- From our ceo (3)
- Software releases (23)
- Education (5)
- People focus (3)
- Types of therapy (1)
- Uncategorized (1)
- Massagebook (36)
- Massage therapy (4)
- Massage practice (1)
- Massagebook (1)
- Fun (1)
- Guest blog (1)
- Resources (2)